Many people think of serotonin as the brain’s “happy chemical”, but what happens when you have too much of a good thing? About 13% of adults in the United States are on antidepressant medications, such as SSRIs. An SSRI, or selective-serotonin reuptake inhibitor, is used to treat symptoms of depression and anxiety by preventing serotonin removal from the brain. Even though SSRIs are widely used, many people are unaware of their potentially dangerous interactions with other drugs. In particular, MDMA, also known as “Molly” or “Ecstasy”, highly interacts with SSRIs and can cause life threatening side effects. By learning about how these two substances work in the brain, we can bring awareness to the risks of serotonin syndrome.
Serotonin does more than just increase our happiness. This neurotransmitter is organically produced by the body, and plays a role in mood, hunger, memory, and even your gastrointestinal system. We understand that a lack of serotonin can lead to issues like depression and anxiety, but it is less often mentioned that too much serotonin can have negative impacts as well. Serotonin syndrome occurs when the brain is unable to keep up with the rapid release and removal of serotonin. The brain is fine tuned to regulate a complex feedback system of many neurotransmitters. When a neuron becomes activated, it sends its serotonin messenger molecules out into the brain. Serotonin then binds to a receptor that is specifically designed to fit with the molecule. Binding then causes a cascade of signals that results in serotonin’s influence on behavior. In order to maintain the brain’s desired balance, SERT (serotonin reuptake transporter) removes serotonin from the receptor and recycles it for later use.
Certain drugs have the ability to affect the amount and type of neurotransmitters that are released. MDMA possesses a unique ability to act as a stimulant and a psychedelic, causing feelings of extreme euphoria, energy, and hallucinations. Other names for MDMA include “Molly” or “Ecstasy”, and is commonly used recreationally. When MDMA is used, it rapidly overwhelms the brain with signals to release more serotonin. More neurotransmitters means more opportunities to bind to receptors, creating lots of activation all at once. Essentially, your brain begins to fire on all cylinders. This leads to the overwhelming emotions that are associated with MDMA consumption. The desired balance of serotonin needed has to be considered when mixing two or more substances. Both MDMA and SSRIs work in different ways to increase serotonin, so taking them together may cause complications.
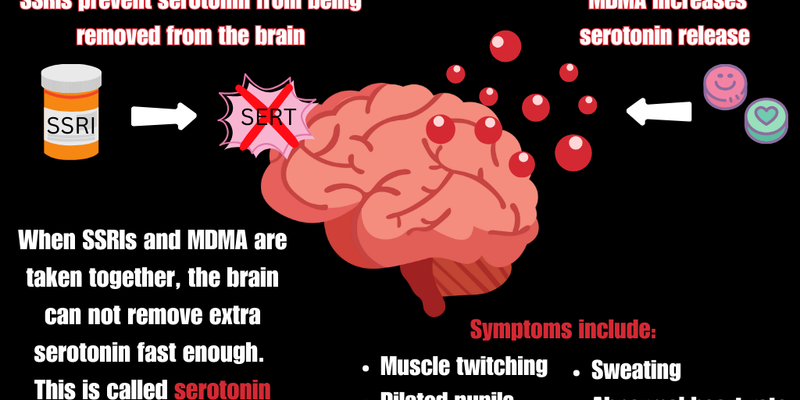
SSRI medications block the removal of serotonin, but MDMA increases serotonin release. The combination of these substances causes a mass release of serotonin, but inhibits its removal. For example, imagine that you are trying to find a place to park in a crowded lot. Almost every spot is taken, and no one seems to be leaving anytime soon. You have no other option but to make your own spot, and parallel park next to a curb. More cars file in, and start parking in the middle of the street or blocking in other cars. Now, no spots are available and other cars are unable to leave the lot. This example mirrors the effects of MDMA and SSRIs when they are both present in the brain. Serotonin has no spot to park in, but also has no way of leaving the lot. The brain is then sent into serotonergic overdrive, causing serotonin syndrome. Symptoms can range from minorly impairing, to extremely life threatening. When too much serotonin gets stuck in the brain, a person can have symptoms of rapid heart rate, dilated pupils, tremor, seizures, and unconsciousness. These symptoms can range from mild, moderate, and severe. Typically, within 24 to 72 hours the brain starts to slowly restore its natural balance. Don’t worry, this is very different from an overdose, and can be reversed and treated by a doctor! It is important to note that naloxone will not be effective in treating serotonin syndrome, since it functions in a different biological system than opioids do. If you are curious about the potential of prescription and recreational drug interactions, talk to your provider about your concerns!
Sources:
Bamalan OA, Moore MJ, Al Khalili Y. Physiology, Serotonin. [Updated 2023 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545168/
Begum, Jabeen, 2024. WebMD. SSRIs: Uses, Benefits, and Side Effects https://www.webmd.com/depression/ssris-myths-and-facts-about-antidepressants
Mayo Clinic, 2024. Serotonin Syndrome. https://www.mayoclinic.org/diseases-conditions/serotonin-syndrome/symptoms-causes/syc-20354758#
Wang et al., 2016. Cleveland Clinical Journal of Medicine. Serotonin Syndrome: Preventing, Recognizing, and Treating It. https://www.ccjm.org/content/83/11/810